Facial paralysis can come on suddenly (in the case of Bell’s palsy, for example) or happen gradually over a period of months (in the case of a head or neck tumour). Depending on the cause, the paralysis might last for a short or extended period of time.
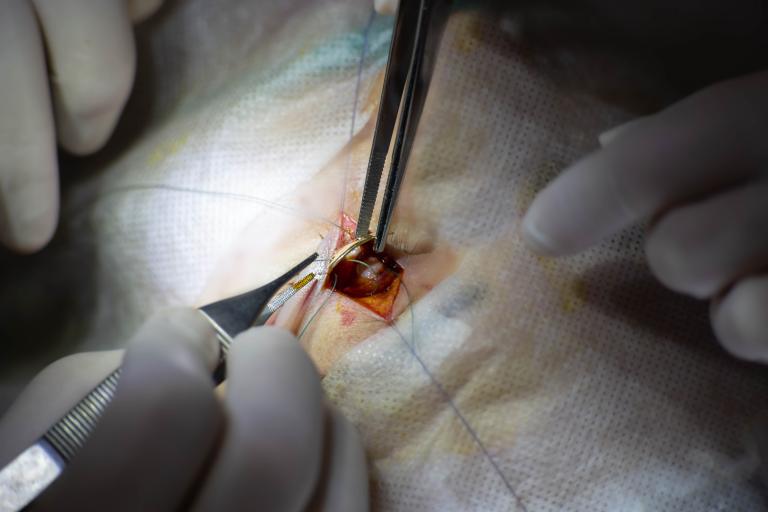
Reconstructive plastic surgery may of help correcting eyelids that won’t fully close or a crooked smile.
Facial paralysis due to other causes may benefit from surgery to repair or replace damaged nerves or muscles, or to remove tumours. Small weights may also be surgically placed inside the upper eyelid to help it close.
Some people may experience uncontrolled muscle movements in addition to paralysis. Botox injections that freeze the muscles, as well as physical therapy, can help.